Conditions and their Treatment - Eating Disorders Brisbane
What are Eating Disorders?
Eating disorders are moderate to severe mental health conditions which are often accompanied by moderate to severe medical issues. Eating disorders are characterised by disturbances in behaviour and thinking around food, eating, weight and/or shape.
Eating disorders do not discriminate. They can affect people of both genders; of all ages, shapes, and sizes; and from all cultural backgrounds. They are serious, potentially-life threatening, and are not a lifestyle choice.
Eating disorders are classified into different diagnoses, depending on the kind of symptoms and frequency of behaviours.
You can’t tell whether or not someone has an eating disorder by looking at them as eating disorders affect people of all ages, genders, sizes, and cultural backgrounds.
People do not simply “grow out” of an eating disorder. In fact, left untreated, eating disorders can have severe consequences for the individual and their loved ones at a physical, emotional, social, and vocational level.
It can be difficult for people to acknowledge, understand and challenge their eating disorder. But with the right support and professional help by specialists in this area, it is entirely possible for a person to achieve complete recovery from their eating or body-image concern.
Our caring professionals have specialist training and experience in the successful treatment of eating disorders, helping people to develop a healthy relationship with food and their body in a safe, non-judgmental environment.
Anorexia Nervosa (AN)
Restriction of energy intake relative to an individual’s requirements, leading to a significantly low body weight in the context of age, sex, developmental trajectory and health status.
Note: Being within the ‘healthy weight’ BMI range does not exclude someone from having Anorexia Nervosa.
Undue influence of body shape and weight on self-evaluation, disturbance of body image, an intense fear of gaining weight, lack of recognition of the seriousness of the illness and/or behaviours that interfere with weight gain are also present.
Most people with anorexia nervosa should be managed on an outpatient basis with psychological treatment provided by a service that is competent in giving that treatment and assessing the physical risk of people with eating disorders.
Cognitive Behavioural Therapy for Eating Disorder (CBT-E) is effective for the treatment for eating disorders in adults. CBT-E addresses the behaviours, thoughts, and emotions associated with an eating disorder. It involves establishing regular eating patterns, reducing rigid dieting, minimising triggers, reducing weight and shape concerns, and improving body image and self-esteem.
Treatment involves 20-40 sessions (depending on severity). Session are initially conducted weekly but then spread out to fortnightly as the client nears recovery.
Maudsley Model of Anorexia Nervosa Treatment for Adults (MANTRA) is a cognitive-interpersonal treatment method which has demonstrated good treatment outcomes in adults with severe and chronic anorexia nervosa.
Treatment is tailored to the specific individual and can include strategies aimed at addressing thinking styles, emotional and relational styles, beliefs about one’s identity as well as the utility of anorexia, and interpersonal relationships.
It consists of 20–40 individual weekly sessions (depending on illness severity), together with 4 or 5 follow-up sessions which are more spread out (monthly).
Anorexia Nervosa is an illness that involves the restriction of food intake relative to one’s requirements, leading to a body weight that is significantly low for the individual.
People with Anorexia Nervosa often experience:
- a sense of self-worth that is largely (even, exclusively) influenced by their ability to control their eating behaviour and body weight/shape,
- an intense fear of gaining weight, and
- an inability to recognition the seriousness of their illness.
Note: Being above or within the ‘healthy weight’ BMI range does not exclude someone from having Anorexia Nervosa.
We understand it’s not easy to admit to yourself or others that you or someone you love may be struggling with concerns such as these however it is important that if you suspect this is an issue, that you seek guidance and support from a professional as soon as possible. Anorexia Nervosa has the highest mortality rate of all mental illness.
As such, we encourage anyone dealing with concerns around eating and/or their body-image to seek help as quickly as possible.
Bulimia Nervosa (BN)
Binge eating (eating a large amount of food in a relatively short period of time with a concomitant sense of loss of control) with purging/compensatory behaviour (e.g. self-induced vomiting, laxative or diuretic abuse, insulin misuse, excessive exercise, diet pills) once a week or more for at least 3 months.
Disturbance of body image, an intense fear of gaining weight and lack of recognition of the seriousness of the illness may also be present.
Cognitive behaviour therapy for bulimia nervosa (CBT-BN), a specifically adapted form of CBT, should be offered to adults with bulimia nervosa. The course of treatment should be for 16 to 20 sessions over 4 to 5 months.
- Involves family and/or significant others (where appropriate);
- Is recovery orientated;
- Occurs in the least restrictive (for example, outpatient, rather than inpatient) treatment setting possible;
- Takes a multidisciplinary, collaborative approach;
- Utilises evidence-based therapies.
Bulimia Nervosa is categorised by episodes of binge eating (eating a large amount of food in a relatively short period of time whilst experiencing a sense of loss of control) followed by inappropriate compensatory behavior (for example, self-induced vomiting or laxative abuse).
Individuals with Bulimia Nervosa also tend to overvalue the importance of controlling their eating behaviour and weight, experience body image disturbance, and have an intense fear of weight gain.
We understand it’s not easy to admit to yourself or others that you or someone you love may be struggling with concerns such as these however it is important that if you suspect this is an issue, that you seek guidance and support from an experienced professional as soon as possible. Although we understand that you might be experiencing a lot of shame around your concerns, our practitioners are warm, caring, and non-judgmental. They understand that you’re not to blame and they’re here to help you overcome your eating disorder one step at a time.
If you or someone you know are struggling with concerns, such as Bulimia Nervosa, we urge you to seek professional support. Left untreated, Bulimia Nervosa can lead to long-term, irreversible health complications.
The team at CFIH work in a collaborative manner, ensuring everyone involved in your care (both within and external to CFIH) communicates regularly and is on the same page. We view you and your loved ones as an integral part of the treatment process. As such, therapy will first seek to develop a shared understanding of your concerns as well as your treatment goals.
Your medical stabilisation is major priority of treatment. We will seek to ensure you are monitored closely by a Medical Practitioner to minimise the need for hospitalisation.
Once you are medically stable, treatment will involve supporting you to achieve and sustain a pattern of eating as well as a weight that is healthy for you. From there, therapy will progress to explore your emotional concerns, both directly and indirectly related to your eating disorder.
Our professionals draw upon evidence-based approaches to treatment, including Family-based therapy (FBT), Cognitive Behavioural Therapy – Enhanced (CBT-E) and the Maudsley model of Anorexia Nervosa treatment for adults (MANTRA).
Your treating team will aim to involve your loved ones in treatment (where appropriate) and/or link you in with additional supports so as to ensure you have support between sessions.
Family-based therapy (FBT) has been demonstrated to be the most effective treatment for Anorexia Nervosa and Bulimia Nervosa in children and adolescents.
This approach actively involves parents in the child’s recovery through supporting parents to help their child restore their weight, reverse malnutrition, and re-learn healthy eating behaviours.
On average, treatment is conducted within 15-20 treatment sessions over a period of approximately 12 months.
Binge Eating Disorder (BED)
Binge eating, in the absence of compensatory behaviour, once a week for at least 3 months. Binge eating episodes are associated with: eating rapidly, when not hungry, until extreme fullness, and/or associated with depression, shame or guilt.
BED is categorised by episodes of binge eating; eating a large amount of food in a relatively short period of time whilst experiencing a sense of loss of control over eating. Unlike Bulimia Nervosa, individuals with BED do not partake in inappropriate compensatory behaviours (such as self-induced vomiting or laxative abuse).
Binge eating episodes are associated with eating rapidly, when not hungry, in secret, until extreme fullness, and are often associated with emotions such as depression, shame and/or guilt.
BED is not something to be embarrassed about. It is a mental health condition. It is not your choice, not your fault, nor something you can control or simply get over. With support of an experienced professional however, full recovery is possible.
The most effective evidence-based treatment method for BED is Cognitive Behavioural Therapy-Enhanced (CBT-E). This approach focuses on restoring regular eating, eliminating episodes of binge-eating, reducing distress surrounding weight and shape, and learning effective emotional regulation skills.
The primary goal of BED treatment is to resolve the eating disorder symptoms as follows:
- Abstinence from binge eating;
- Reduction of weight and shape related concerns; and
- Weight stabilisation.
Weight-loss is not a part of treatment of BED. If there are concerns about the individual’s health, these concerns will be addressed through lifestyle and behaviour changes (such as increased physical activity and improved nutrition).
While treatment with an experienced therapist is always recommended as the first line approach, there is also evidence of Guided-Self Help (GSH) approaches being successful in achieving sustained recovery.
Overcoming Bulimia and Binge-Eating: A self-help guide using Cognitive Behavioral Techniques. Rev Ed. Auth: Peter Cooper Pub: Robinson UK, 2009
Contrary to popular misconception, eating disorders are not lifestyle choices. They are serious and debilitating illnesses that negatively affect a person’s emotions, thoughts, and behaviours around food, eating, exercise, and body-image.
Other Conditions and Treatments
Although not yet a formally-recognised diagnosis, the notion of ‘Orthorexia’ is certainly a very real and concerning one. Literally meaning “fixation on righteous eating,” those with Orthorexia are described as being obsessed with healthy eating.
With all the hype about gluten-free, dairy-free, sugar-free, organic, grain-free, it’s no wonder that many are left feeling guilty no matter what they consume. Its tendency to be a common and wide-spread phenomenon does not mean it doesn’t warrant specialist treatment.
In addition to deleterious effects on mental health, Orthorexia can negatively impact physical health through its tendency to lead to Anorexia Nervosa, binge eating (a commonly occurring side-effect of overly restrictive eating), purging, and malnutrition.
While there is nothing wrong with wanting to improve your health through making more nutritious choices, a focus on health that does not include mental health and social relationships is not healthy at all.
Just because a person’s disordered eating behaviours and symptoms doesn’t exactly match those of a listed eating disorder, it by no means is any less serious or less worthy of receiving professional help.
Disordered thoughts/feelings/behaviours concerning food and weight/shape that does not meet full criteria for one of the above categories, but has specific disordered eating behaviours such as restricting intake, purging and/or binge eating as key features.
Eating disorders are complex illnesses and not everyone will experience the same behaviours, symptoms and emotions. If a person is suffering from disordered thoughts, feelings or behaviours concerning food and/or weight and shape, it is important that they get the support they deserve.
For further guidance and information, please feel free to reach out to our team for a obligation-free 15-minute phone consultation.
Significant weight loss, nutritional deficiency, dependence on nutritional supplement or marked interference with psychosocial functioning due to caloric and/or nutrient restriction, but without weight or shape concerns.
ARFID is defined by a disturbance in eating that results in a failure to meet the nutritional or energy needs a person leading to:
- weight loss or failure to gain weight as expected;
- nutritional deficiencies;
- a dependence on enteral feeding or food supplements; and/or
- an impairment in psychosocial functioning (e.g. it negatively impacts on the individual’s social life).
This avoidance may be due to a lack of interest in food, concerns about consequences of eating (such as a fear of choking or vomiting), or the displeasure experienced with the tastes and/or textures of foods. Unlike other eating disorders, individuals diagnosed with ARFID do not experience disturbances in body-image and/or a fear of weight gain.
To be diagnosed with ARFID, the avoidance of food must not be explained by:
- normal culture practices;
- food allergies;
- another eating disorder.
Unlike typical picky eating experienced early in childhood, people do not outgrow ARFID without specialist and targeted treatment. Due to the negative impact ARFID can have on an individual’s physical, emotional, and social health, we urge you to speak to a trained professional in the field if you suspect that you or someone you know might be experiencing ARFID.
Selective or “Fussy” Eating in Children
Across all cultures, enjoying a meal can represent more than simply consuming our daily nutrient requirements. Food can bring people together, celebrate an occasion, convey our feelings and is an important aspect of many cultural and religious identities. However, for some families, meal times represent a battleground of distress, avoidance and anxiety when children have selective eating.
Approximately one in four children experience eating problems during early childhood, with one in two families stating that their child actively avoids particular foods. These difficulties are present in some children from birth and infancy, whilst other children develop eating difficulties related to environmental or psychological triggers.
Eating problems are a common challenge for many parents. However, when these behaviours are accompanied by physical health, behavioural or emotional problems or are causing significant distress to the child or parent, it is important for them to seek support and for a diagnosis of Avoidant and Restrictive Food Intake Disorder (ARFID) to be ruled out.
Without intervention, insufficient nutrient consumption can lead to delays in motor skills, speech and language development, as well as stress and mental health difficulties.
Children with eating difficulties are usually restricted in either:
- The variety of foods consumed (typical description of picky eaters);
- The quantity of foods consumed (including appetite issues, lack of interest, avoiding eating);
- The texture of foods consumed (e.g. children only eating pureed or chewy foods).
By the time many families present for treatment, meal times are well established as a negative experience for both parents and children. Children have often developed an intense fear of foods and can become highly distressed at the sight or suggestion of new foods.
Behavioural family interventions are the most effective approaches to the treatment of child feeding problems. This involves helping parents to alter the family’s feeding practices to promote improvements in their child’s eating behaviours.
Here are our top 5 tips for helping your child with their picky or selective-eating habits.
Our priority is to get you the right treatment individually tailored. As such, our psychologists are trained and highly skilled in a number of therapies and treatment approaches. Our treatment options include:
- CBT (Cognitive Behaviour Therapy)
- ACT (Acceptance and Commitment Therapy)
- FBT (Family-Based Therapy)
- DBT (Dialectic Behavioural Therapy)
- Schema Focused Therapy
- Motivational Interviewing
- Play-Based Therapy
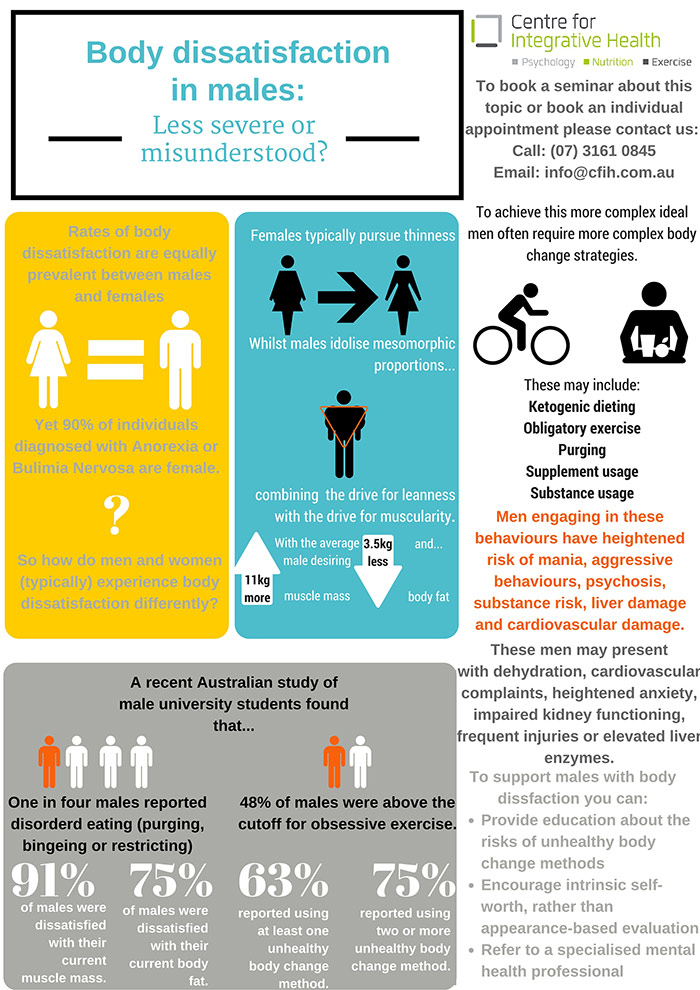
Despite misconceptions, rates of body dissatisfaction among males are approaching similar rates to that among females. While females generally pursue thinness, males typically desire mesomorphic proportions; combining the drive for thinness/leanness as well as the drive for muscularity.
Increasingly more men are resorting to complex and dangerous strategies to achieve body ideals, with the current rates reported to exceed those of Anorexia Nervosa or Bulimia Nervosa. Although it is not currently recognised or identified as an illness, there is help available.
If you, or someone you know, seems to be experiencing body dissatisfaction to a degree that interferes with physical, mental or emotional health, CFIH can offer the support and advice to help.
Our approaches involve improving awareness of eating behaviours, establishing regular eating routines, reducing rigid dieting, eating in response to hunger and satiety, minimising triggers for overeating, developing alternative approaches to managing emotions, and improving body image and self-esteem.
Behavioural family interventions are the most effective approaches to the treatment of child feeding problems.
This involves helping parents to alter the family’s feeding practices to promote improvements in their child’s eating behaviours.
Individuals with weight, shape and body image concerns often experience physical health (e.g., diabetes, polycystic ovary syndrome, sleep apnoea) and emotional health (e.g., depression, anxiety, adjustment disorders) issues.
Optimal treatment involves integrated care that considers physical, psychological, and social aspects of illness.
At CFIH, we are passionate about ensuring our clients get the best possible treatment and that treatment translates to meaningful change.
For this reason, CFIH embraces a Feedback Informed Treatment (FIT) approach, which means that we use data to tell us how each of our clients is progressing. Prior to each session with one of our practitioners, we will ask you to complete the 4-item Outcome Rating Scale (ORS).
We will then monitor, analyse, and report on your progress every step of the way. If treatment is not assisting you, we will will review this with you and offer you alternative treatment approaches.
Nine Truths about Eating Disorders
Truth #1: Many people with eating disorders look healthy, yet may be extremely ill.
Truth #2: Families are not to blame, and can be the patients’ and providers’ best allies in treatment.
Truth #3: An eating disorder diagnosis is a health crisis that disrupts personal and family functioning.
Truth #4: Eating disorders are not choices, but serious biologically influenced illnesses.
Truth #5: Eating disorders affect people of all genders, ages, races, ethnicities, body shapes and weights, sexual orientations, and socioeconomic statuses.
Truth #6: Eating disorders carry an increased risk for both suicide and medical complications.
Truth #7: Genes and environment play important roles in the development of eating disorders.
Truth #8: Genes alone do not predict who will develop eating disorders.
Truth #9: Full recovery from an eating disorder is possible. Early detection and intervention are important.
Produced in collaboration with Dr. Cynthia Bulik, PhD, FAED, who serves as distinguished Professor of Eating Disorders in the School of Medicine at the University of North Carolina at Chapel Hill and Professor of Medical Epidemiology and Biostatistics at the Karolinska Institutet in Stockholm, Sweden. “Nine Truths” is based on Dr. Bulik’s 2014 “9 Eating Disorders Myths Busted” talk at the National Institute of Mental Health Alliance for Research Progress meeting.
The earlier that appropriate treatment is sought, the greater the chance of full recovery. If you think you, or someone you know, might be struggling with an eating disorder or weight concern, our team of professionals are here to support you.
You can find out more about overcoming eating disorders and weight concerns by contacting us for a free 15-minute consultation. We are always open to discussing your concerns as well as the ways in which we might support you.